A new gene therapy approach appears to avoid toxicity to the dorsal root ganglion (DRG), an unique cluster of sensory neurons, seen in non-human primates during gene therapy studies for neurological disorders, researchers report, by taking advantage of a natural process of gene silencing.
The approach successfully protected the DRG of the primates from the introduced gene’s excessive activity known as a transgene, and subsequent toxicity without affecting the activity of the transgene elsewhere in the nervous system.
After spinal canal injection of AVXS-101, approved as Zolgensma when given as an intravenous infusion, DRG inflammation and toxicity were observed in non-human primates, prompting a partial hold of a Phase 1/2 trial (NCT03381729) to allow for further investigation. This trial, called STRONG, is testing the intrathecal (spinal canal) injection of this gene therapy in children aged 6 months to 5 years with spinal muscular atrophy (SMA).
The study, “MicroRNA-mediated transgene expression inhibition reduces dorsal root ganglion toxicity in primates through AAV vectors,” was published in the journal Science Translational Medicine.
Juliette Hordeaux, PhD, the first author of the study at the Perelman School of Medicine (Penn Medicine) at the University of Pennsylvania, said in a press release, “We believe that this new approach could universally improve safety in gene therapy,” as well as in SMA.
Hordeaux, who is also senior director of translational research for the gene therapy program of Penn Medicine, added, “This approach could be used to design other gene therapy [carriers] to repress transgene [activity] in the cell types that are affected by toxicity and not others, which is critical because you need [such activity] everywhere else to effectively treat the disorder.”
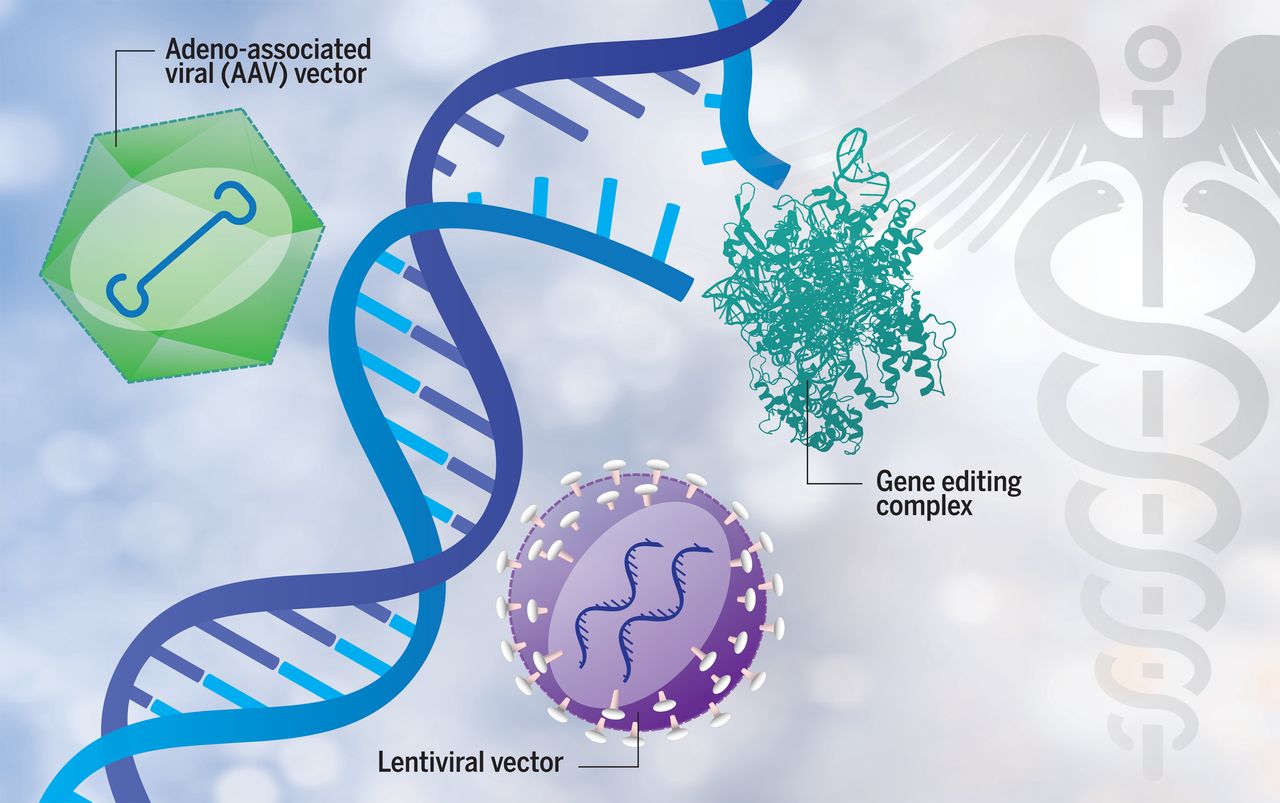
In order to correct or replace a faulty gene within specific cells in the body, gene therapy works to provide a functional version of a gene. A modified and harmless adeno-associated virus (AAV) is used by most treatment approaches today as a’ carrier’ for the working gene, a vehicle to transport it to a target cell.
But previous studies, including primate work by Penn researchers, have shown that central nervous system (CNS; brain and spinal cord) gene therapies based on AAV can damage DRG, a cluster of spinal nerve neurons that carry sensory information from the periphery to the spinal cord.
Notably, in studies, DRG toxicity was observed regardless of the route of administration of the therapy (directly into the bloodstream or spinal canal). No reports are known of such toxicity in humans, including infants treated with STRONG.
In preventing this toxicity, conventional immunosuppressive regimens were ineffective, strongly indicating that their cause was not an excessive immune response. This led Hordeaux and her colleagues from Penn to assess whether the damage was associated with excessive transgene product levels, which could cause cellular stress.
They took advantage of RNAi, a natural gene silencing process in which microRNA (miR) molecules bind to a particular messenger RNA (mRNA), targeting it for destruction and preventing the production of that protein, to test their idea. (The molecule derived from DNA and used as a protein production template is mRNA.)
Since the miR183 complex is specifically produced in sensory tissues and organs, such as the dorsal root ganglion, at the end of the transgene sequence in an AVV, the researchers introduced the sequence targets of miR183. Any mRNA produced from the transgene would thus be destroyed by the naturally present miR183 in DRG neurons, preventing the production of protein in these cells.
Researchers then compared the effects of AAV administration with a transgene containing or not containing the sequence targets of miR183 in non-human primates’ cerebrospinal fluid (the fluid that bathes the brain and spinal cord).
In contrast, steroids given to primates treated with unmodified AAVs, despite their known anti-inflammatory and immunosuppressive effects, failed to alleviate DRG harm. The researchers wrote that this ineffectiveness was “consistent with the proposal that immune system activity does not mediate this neuronal toxicity.”
“In most of our [non-human primate] studies, we were concerned about the DRG [toxicity] that was observed,” said James M. Wilson, MD, PhD, senior author of the study, and director of the gene therapy program and professor of medicine and pediatrics at Penn Medicine.
“This modified [viral] vector shows great promise to reduce DRG toxicity and should make it easier for many CNS diseases to develop safer AAV-based gene therapies,” Wilson added.
Novartis gene therapy Zolgensma, when given directly into the bloodstream, is currently available in the United States and Japan for use in newborns and infants up to 2 years of age with any type of SMA, and in Europe for those with almost all types weighing up to 21 kilograms (about 46 pounds).
In order to meet a U.S. Novartis plans to launch a new AVXS-101 IT trial with the Food and Drug Administration (FDA) request for a ‘pivotal confirmatory study’ of the use of gene therapy in older SMA patients treated by intrathecal (IT) injection.
This administration route is favored for those beyond toddler age, as it is thought to better target the motor neurons damaged by the disease.
According to the firm, until the hold on STRONG is lifted, this IT trial may not include U.S. sites.
Source- smanewstoday.com